Located in Sector 51 Gurugram, it brings together expert care in Orthopaedics,Eye , and Physiotherapy doctors to provide complete health solutions under one roof.
- Advanced Technology
- Expert Professionals
- Personalized Care
- On Time Treatment
- 10+ Years of Experience
About Us
Welcome to GS CARE MULTISPECIALITY CLINIC
Best Multispeciality Clinic in Gurgaon for Ortho Eye Physiotherapy services
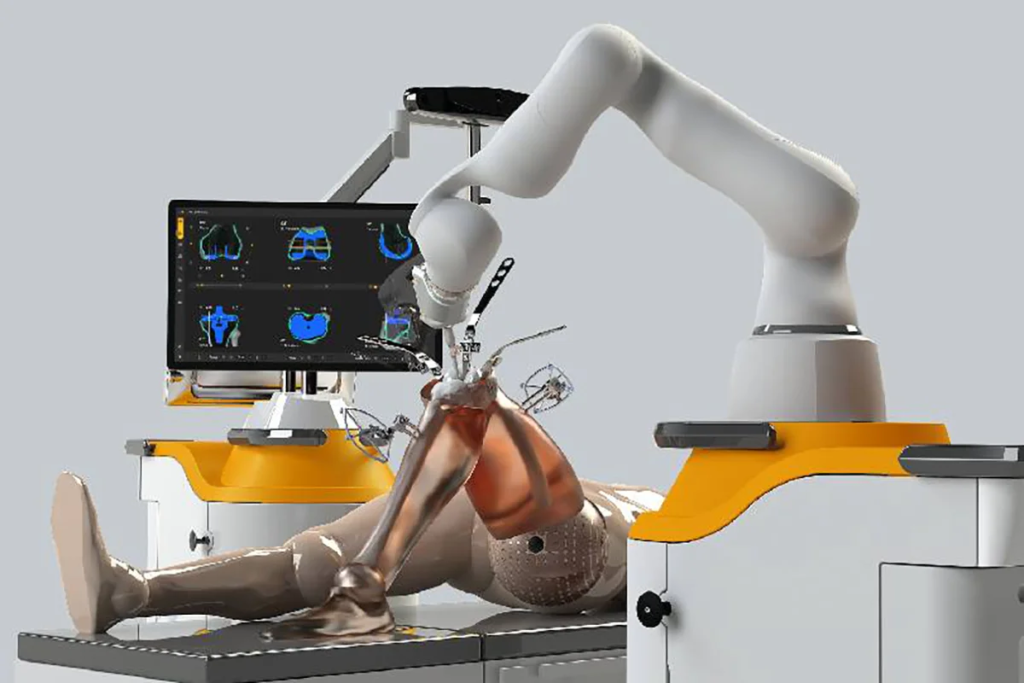
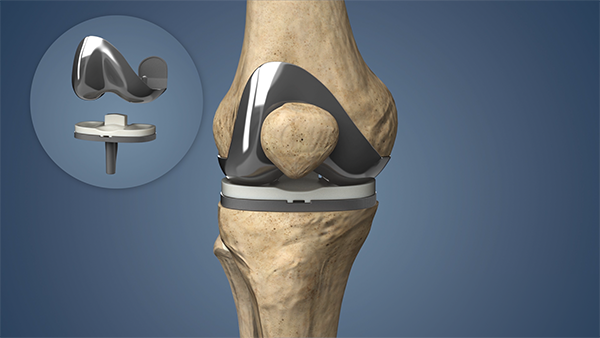
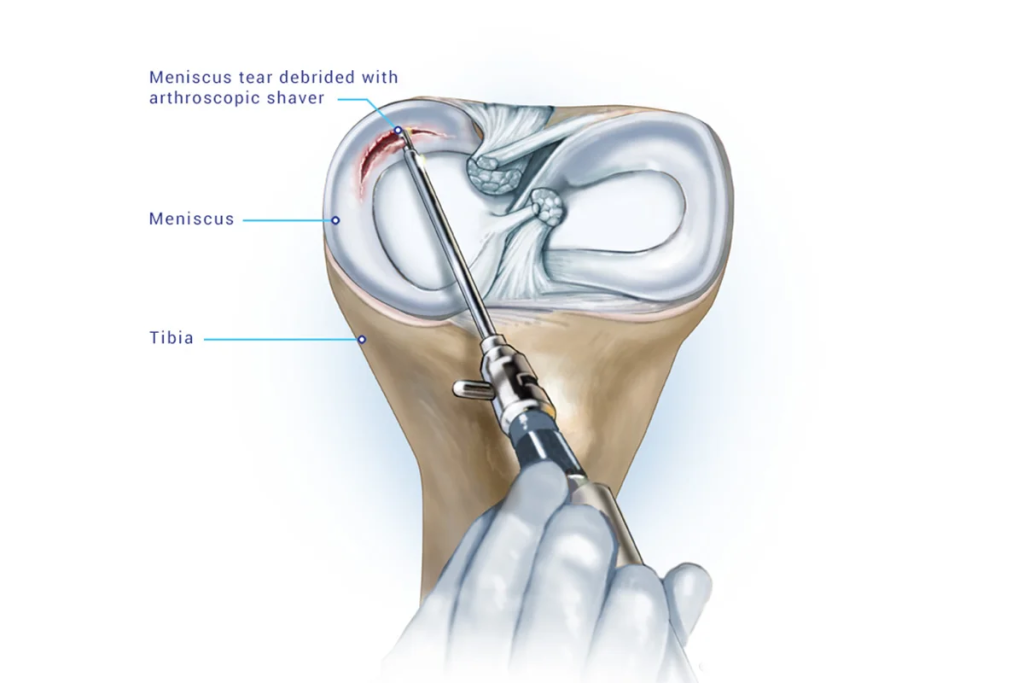
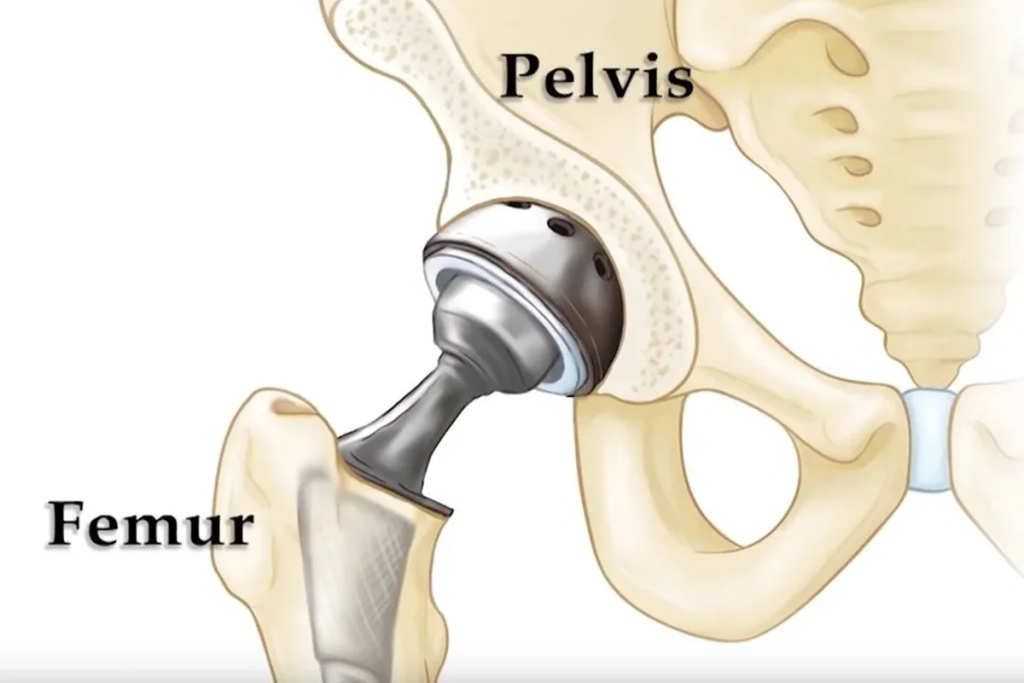
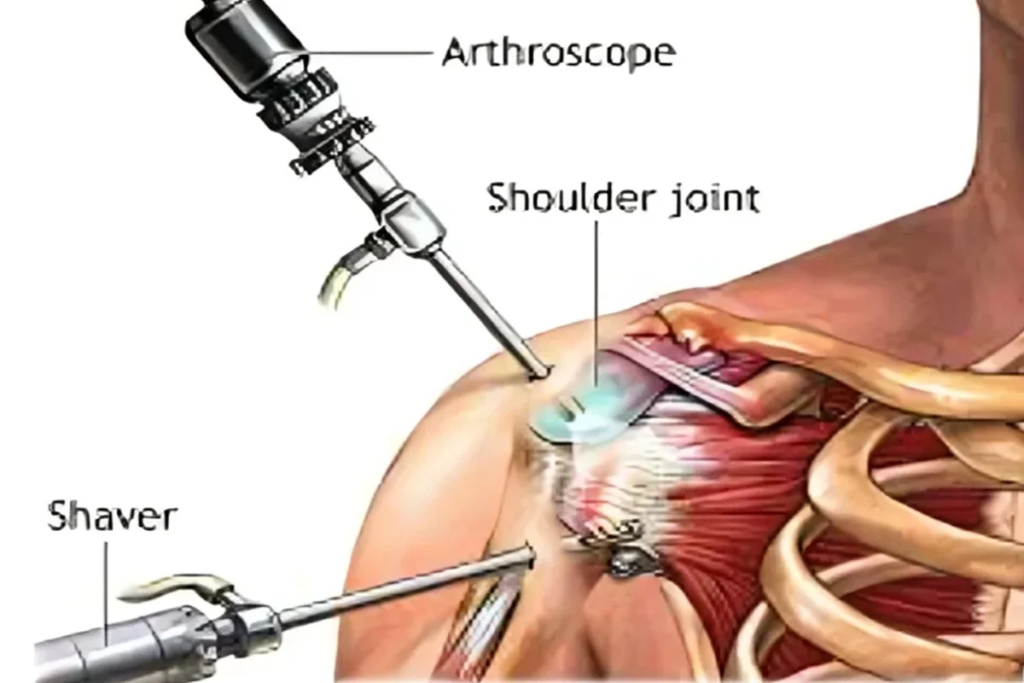
Located in Sector 51 Gurugram, it brings together expert care in Orthopaedics,Eye , and Physiotherapy doctors to provide complete health solutions under one roof. Our Eye Care department offers everything from routine eye check-ups and advanced diagnostics to the management of cataracts, glaucoma, diabetic eye disease, and all other eye and vision-related conditions, along with a wide range of stylish and comfortable spectacles and lenses to suit every need. The Orthopaedics unit specializes in the treatment of bones, joints, muscles, and spine problems—covering fractures, arthritis, sports injuries, back pain, and complex joint replacement surgeries including robotics—with the goal of restoring mobility and relieving pain. Complementing this, our Physiotherapy and Rehabilitation department provide personalized programs for post-surgical recovery, chronic pain management, sports injury rehabilitation, neurological care, and preventive wellness, using modern techniques to help patients regain strength, flexibility, and independence. In addition to these core specialties, we also offer Apollo Blood Tests and comprehensive eye care solutions for preventive health support. With a team of skilled specialists, state-of-the-art facilities, and a patient-first approach, GS Multispeciality Clinic Gurugram is dedicated to ensuring healthier lives through compassionate, advanced, and integrated medical care.




Meet Our Doctors

Dr Guruditta Khurana
MBBS, D.ORTHO(Medalist), FIJR(Robotic),
Fellowship in Robotic Joint Replacement Surgery

Dr Sneha T Khurana
MBBS, MS (Ophthalmology) – Medalist

Dr Kajal Sharma
BPT, COMT ,Certified IASTM

DR Nilesh Chakraborty PT
BPT, COMT Certified Cupping and Dry needling Sports Rehab expert
Our Services
Take the first step towards better health. Book your appointment now!
Trustindex verifies that the original source of the review is Google. Gs multi-speciality clinic best service provideTrustindex verifies that the original source of the review is Google. Gs clinic good service provideTrustindex verifies that the original source of the review is Google. Good staffTrustindex verifies that the original source of the review is Google. Very goodTrustindex verifies that the original source of the review is Google. Very good orthopedic doctor in the area
Why Choose US?
- Expert Surgeon: 10+ Years of Experience
- Personalized Care.
- Minimal Recovery, Precise Results
- One Stop solution.